VO2 Max: The Ultimate Predictor of Human Longevity
For decades, the medical establishment has operated under a paradigm of pathology management. The annual physical examination—a ritual embedded in the preventative health infrastructure of the developed world—typically revolves around a specific set of biomarkers: blood pressure, lipid panels (cholesterol, LDL, HDL), fasting glucose, and perhaps inflammatory markers like C-reactive protein. When these numbers deviate from the norm, pharmaceutical interventions are prescribed to force them back within reference ranges. While this approach has undoubtedly extended life expectancy by mitigating acute cardiovascular events, it often fails to address the underlying physiological robustness of the organism. It treats the symptoms of decay rather than preserving the engine of life.
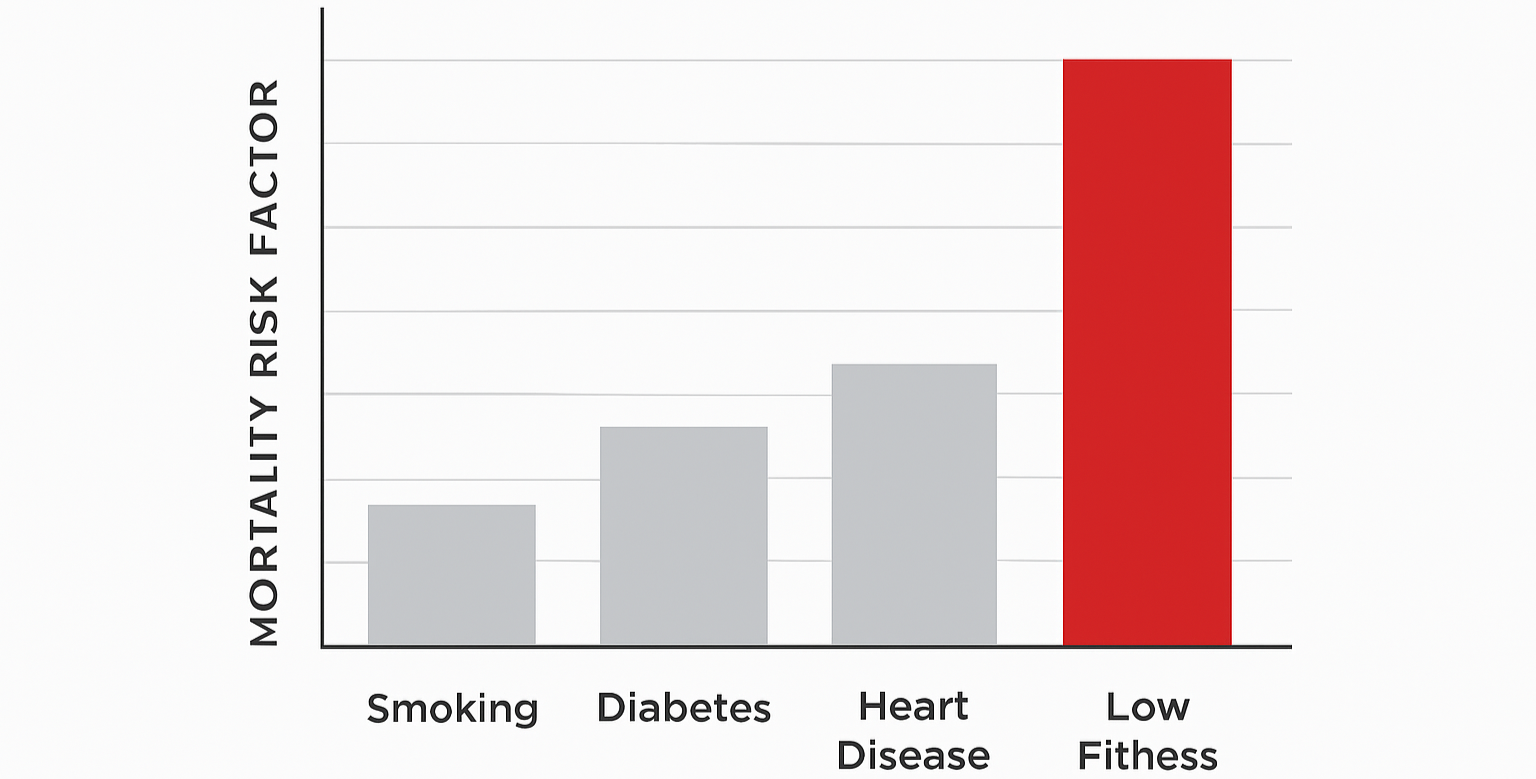
However, a seismic shift is occurring in the fields of longevity science and preventative cardiology. A growing body of evidence, culminating in massive retrospective cohort studies, suggests that there is a single metric that outperforms smoking status, hypertension, high cholesterol, and type 2 diabetes as a predictor of all-cause mortality. That metric is Cardiorespiratory Fitness (CRF), clinically quantified as VO2 Max.
VO2 max, or maximal oxygen uptake, has historically been the domain of elite endurance athletes. It was viewed as a performance metric, a number relevant only to those pinning a race number to their chest. This categorization has proven to be a catastrophic oversight in public health. Recent data indicates that VO2 max is not merely a measure of athletic potential; it is a vital sign that quantifies the functional capacity of the human machine.
The Clinical Evidence – Mandsager et al. and the Mortality Curve
In the hierarchy of clinical evidence, large-scale studies with long-term follow-up provide the data necessary to infer causality and risk. In 2018, a team of researchers at the Cleveland Clinic, led by Dr. Wael Jaber and Dr. Kyle Mandsager, published a study in JAMA Network Open that fundamentally altered our understanding of the relationship between fitness and survival.
Quantifying the Risk of Sedentarism
The study analyzed data from 122,007 patients who underwent exercise treadmill testing. Unlike many fitness studies that rely on self-reported physical activity (which is notoriously unreliable), this study used objective measures. Patients were tested to measure their functional capacity in Metabolic Equivalents of Task (METs).
The results were stark. The analysis revealed an inverse relationship between cardiorespiratory fitness and mortality across all groups. When compared to the "Elite" performers (top 2.3%), those in the "Low" fitness group (the bottom 25%) faced an adjusted hazard ratio (HR) for all-cause mortality of 5.04.
To put this in perspective, low performers were five times more likely to die during the follow-up period than their elite counterparts. The study authors explicitly compared this risk to traditional clinical risk factors, revealing a hierarchy of danger that contradicts standard public perception:
Low Fitness vs. Smoking: Being unfit is ~3.5x riskier than being a current smoker.
Low Fitness vs. Heart Disease: Being unfit is ~3.9x riskier than having Coronary Artery Disease (CAD).
Low Fitness vs. Diabetes: Being unfit is ~3.6x riskier than having diabetes
The "No Ceiling" Phenomenon
Prior to this study, there was a debate regarding the "Extreme Exercise Hypothesis"—the idea that extreme fitness might be cardiotoxic. The Mandsager study effectively debunked this concerning longevity. The data showed no observed upper limit of benefit.
Even compared to "High" performers (75th-97.6th percentile), the "Elite" group still enjoyed a significant survival advantage. This implies that "good" is not enough. The physiological adaptations required to reach the top 2% of the population provide a physiological reserve that is protective against death.
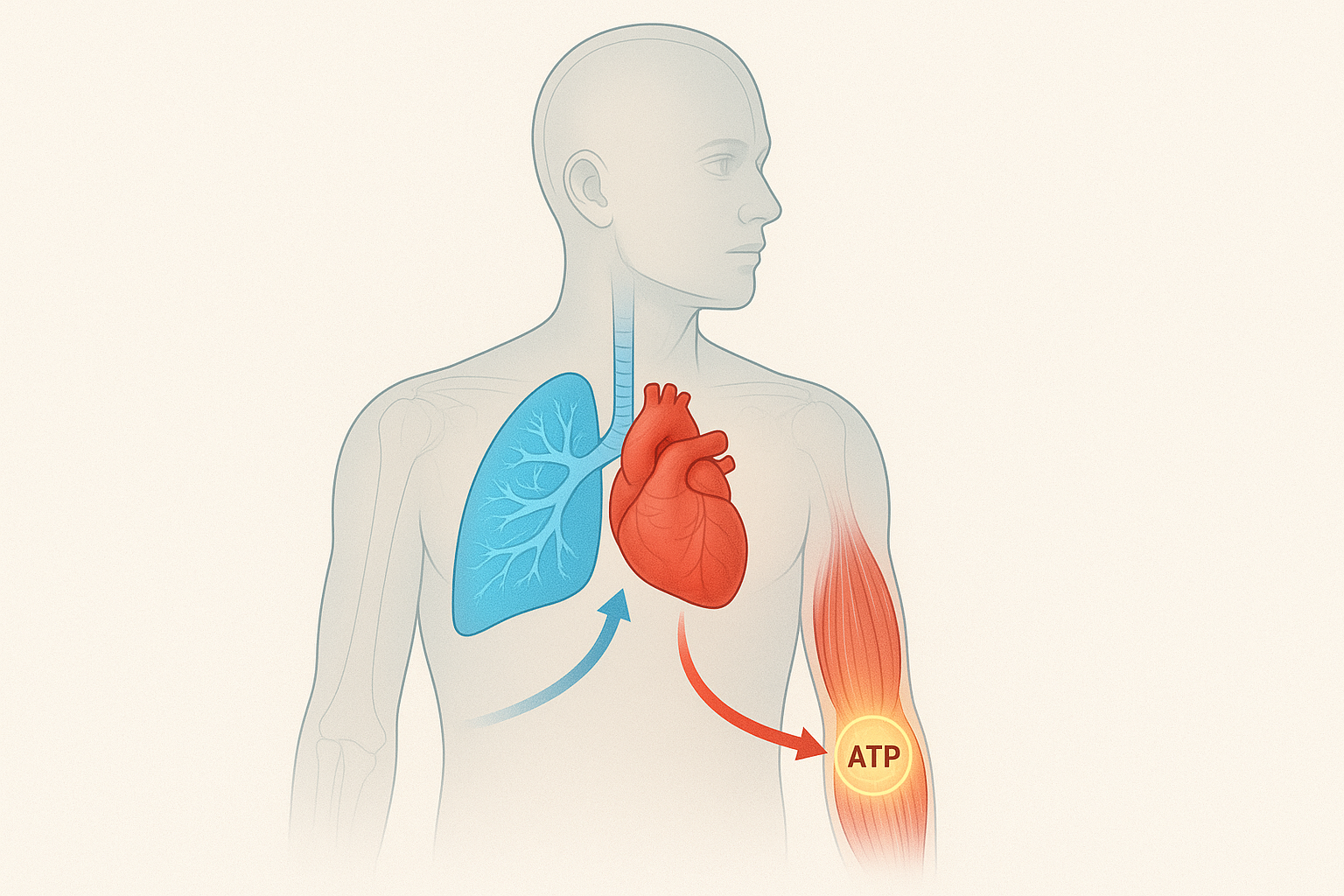
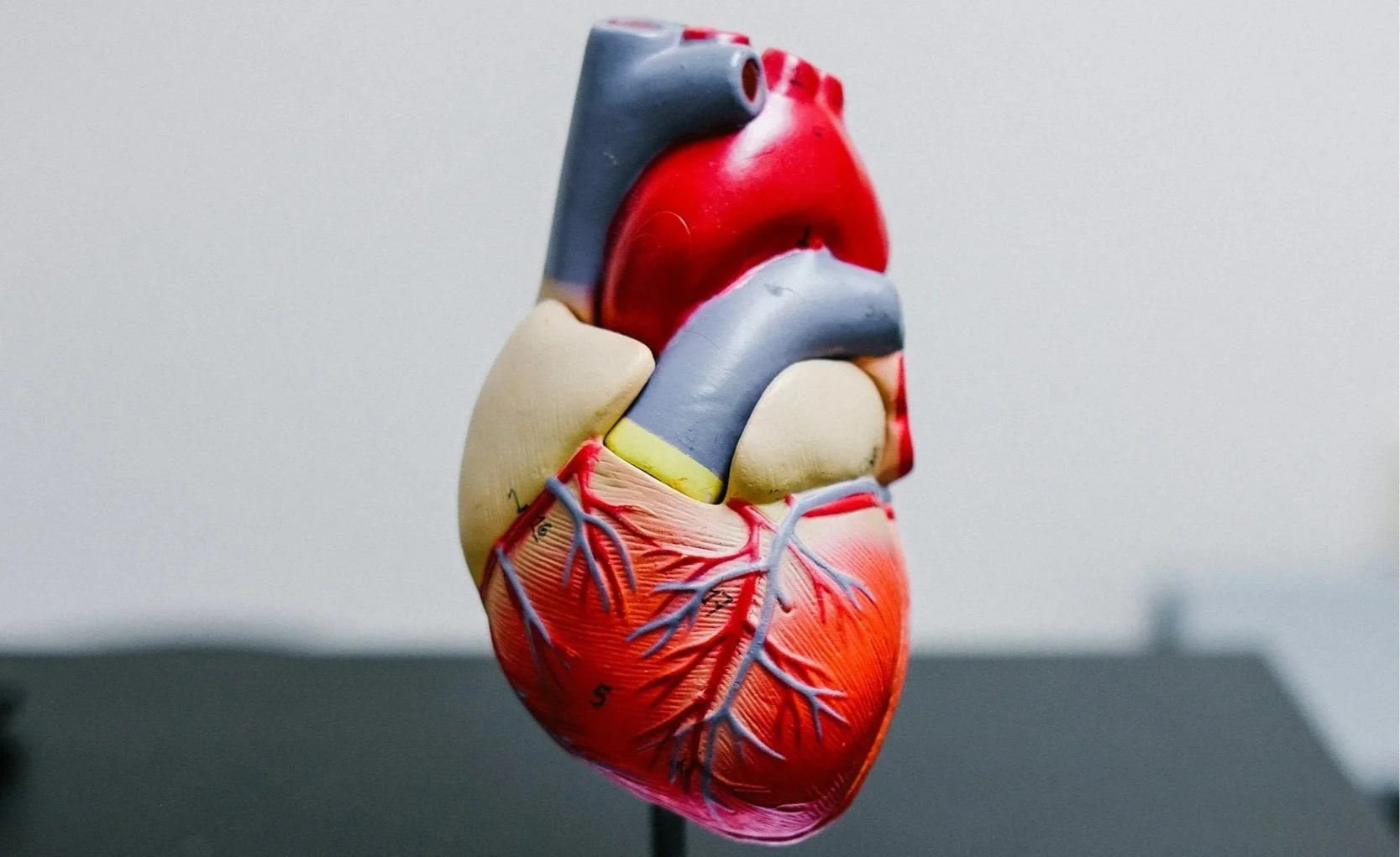
Central Adaptations: The Heart as a Pump
Since maximum heart rate is largely fixed by genetics and age, the primary driver of increased Cardiac Output in elite athletes is Stroke Volume—the amount of blood ejected from the left ventricle with a single beat.
Elite athletes achieve massive stroke volumes through a process called Eccentric Hypertrophy. During high-intensity training, the heart is subjected to volume overload, stretching the chamber walls of the left ventricle. This allows for a greater End Diastolic Volume (EDV)—more blood fills the heart before it pumps—making the heart a more efficient machine.
Peripheral Adaptations: The Metabolic Sink
Delivering oxygen is futile if the muscles cannot extract it.
Capillarization: Endurance training promotes angiogenesis—the growth of new capillary beds surrounding muscle fibers, ensuring oxygen has a short distance to travel.
Mitochondrial Density: The mitochondria are the cellular power plants where aerobic respiration occurs. Exercise triggers PGC-1α, a protein that drives the creation of new mitochondria. High-intensity training also increases the density of cristae, the inner folds where energy is produced.
Building the Elite Engine
The most effective approach, supported by decades of data, is Polarized Training: a combination of high-volume low-intensity training (Zone 2) and specific high-intensity interval training (Norwegian 4x4).
The Foundation: Zone 2 Training
Zone 2 is a metabolic state where fat oxidation is maximal.
The Mechanism: Continuous contraction of Type I (slow-twitch) fibers stimulates AMPK pathways, driving mitochondrial growth. It also improves metabolic flexibility, or the ability to switch between fuel sources efficiently.
Lactate Clearance: Zone 2 increases Monocarboxylate Transporters (MCT1), which shuttle lactate into the mitochondria to be reused as fuel.
The Protocol: 3–4 sessions per week, 45–90 minutes duration. You should be able to speak in full sentences, but not sing.
The Norwegian 4x4 Protocol
To stretch the heart via the Frank-Starling mechanism, one must train at intensities where venous return (blood flowing back to the heart) is maximal.
The Work Interval: 4 minutes at 85–95% of HR max.
The Recovery: 3 minutes active recovery (Zone 2).
Repetition: 4 rounds.
Frequency: 1-2 times per week.
Why it works: The heart spends roughly 10-12 minutes in the optimal remodeling zone, far longer than in short sprints.
Quantification – Measuring the Me
4.1 The Gold Standard: CPET
The most accurate way to measure VO2 max is Cardiopulmonary Exercise Testing (CPET). This laboratory test measures gas exchange breath-by-breath to identify specific Ventilatory Thresholds, providing the precise heart rates needed for training.
Wearable Technology
In the absence of a metabolic cart, modern wearables utilize algorithms (often by Firstbeat Analytics) to estimate VO2 max.
Garmin: Generally considered superior for athletic training due to integration with chest straps and linear tracking with lab results.
Apple Watch: While useful, studies suggest it may underestimate VO2 max in highly fit individuals (Elite) and overestimate it in those with poor fitness.
Product Recommendations – The 2025 Toolkit
To execute these protocols effectively, relying on wrist-based optical sensors is a liability during high-intensity intervals.
Heart Rate Monitors
Polar H10: The gold standard. It utilizes an electrocardiogram (ECG) strip to detect electrical signals directly, making it instantaneous and accurate for 4x4 intervals.
Garmin HRM-Pro Plus: Ideal for data harvesters, capturing running dynamics and offering store-and-forward capabilities.
Wahoo TRACKR: A 2025 entrant featuring a rechargeable lithium-ion battery, solving the waste issue of coin-cell batteries.
Training Watches
Garmin Fenix 8: The 2025 flagship. Rugged, with weeks of battery life, it tracks Heart Rate Variability (HRV) to contextualize recovery.
Coros Pace 3: The value king. Pure data without smartwatch distractions, featuring excellent "EvoLab" training load management.
Conclusion: The Centenarian Athlete
The convergence of the Mandsager mortality data and modern exercise physiology provides a clear roadmap for the future of preventative medicine. We are moving away from a model where "health" is defined as the absence of disease, toward a model where health is defined by the magnitude of functional capacity.
VO2 max is the currency of this capacity. It is a reservoir of physiological resilience. When a 40-year-old trains to increase their VO2 max from "Average" to "Elite," they are not just improving their 10k time; they are banking survival points for their 80s. They are building a heart that can withstand the stress of surgery, a vascular system that can resist hypertension, and a mitochondrial network that can prevent metabolic derangement.
The path is rigorous but simple. It does not require exotic supplements. It requires the discipline of Zone 2 to build the engine's efficiency and the intensity of the Norwegian 4x4 to expand the engine's size. The only limit is the work one is willing to do.
Works Cited
Mandsager, K., Harb, S., Cremer, P., Phelan, D., Nissen, S. E., & Jaber, W. (2018). Association of Cardiorespiratory Fitness With Long-term Mortality Among Adults Undergoing Exercise Treadmill Testing. JAMA Network Open, 1(6), e183605. https://doi.org/10.1001/jamanetworkopen.2018.3605
Levine, B. D. (2008). VO2max: what do we know, and what do we still need to know?. The Journal of Physiology, 586(1), 25–34. https://doi.org/10.1113/jphysiol.2007.147694
Helgerud, J., Høydal, K., Wang, E., et al. (2007). Aerobic high-intensity intervals improve VO2max more than moderate training. Medicine and Science in Sports and Exercise, 39(4), 665–671. https://doi.org/10.1249/mss.0b013e3180304570
San-Millán, I., & Brooks, G. A. (2018). Assessment of Metabolic Flexibility in Elite Athletes and Individuals with Type 2 Diabetes and Metabolic Syndrome. Sports Medicine, 48(2), 467–479. https://doi.org/10.1007/s40279-017-0751-x
Seiler, S. (2010). What is best practice for training intensity and duration distribution in endurance athletes?. International Journal of Sports Physiology and Performance, 5(3), 276–291. https://doi.org/10.1123/ijspp.5.3.276
Suggested Tags
#VO2Max #Longevity #MandsagerStudy #Zone2Training #Norwegian4x4 #ExercisePhysiology #Biohacking #HeartHealth #Mitochondria #Garmin #PolarH10 #PreventativeMedicine #FitnessScience #Cardio #EnduranceTraining