The Resilience Switch: Mastering Stress and Activating Deep Recovery
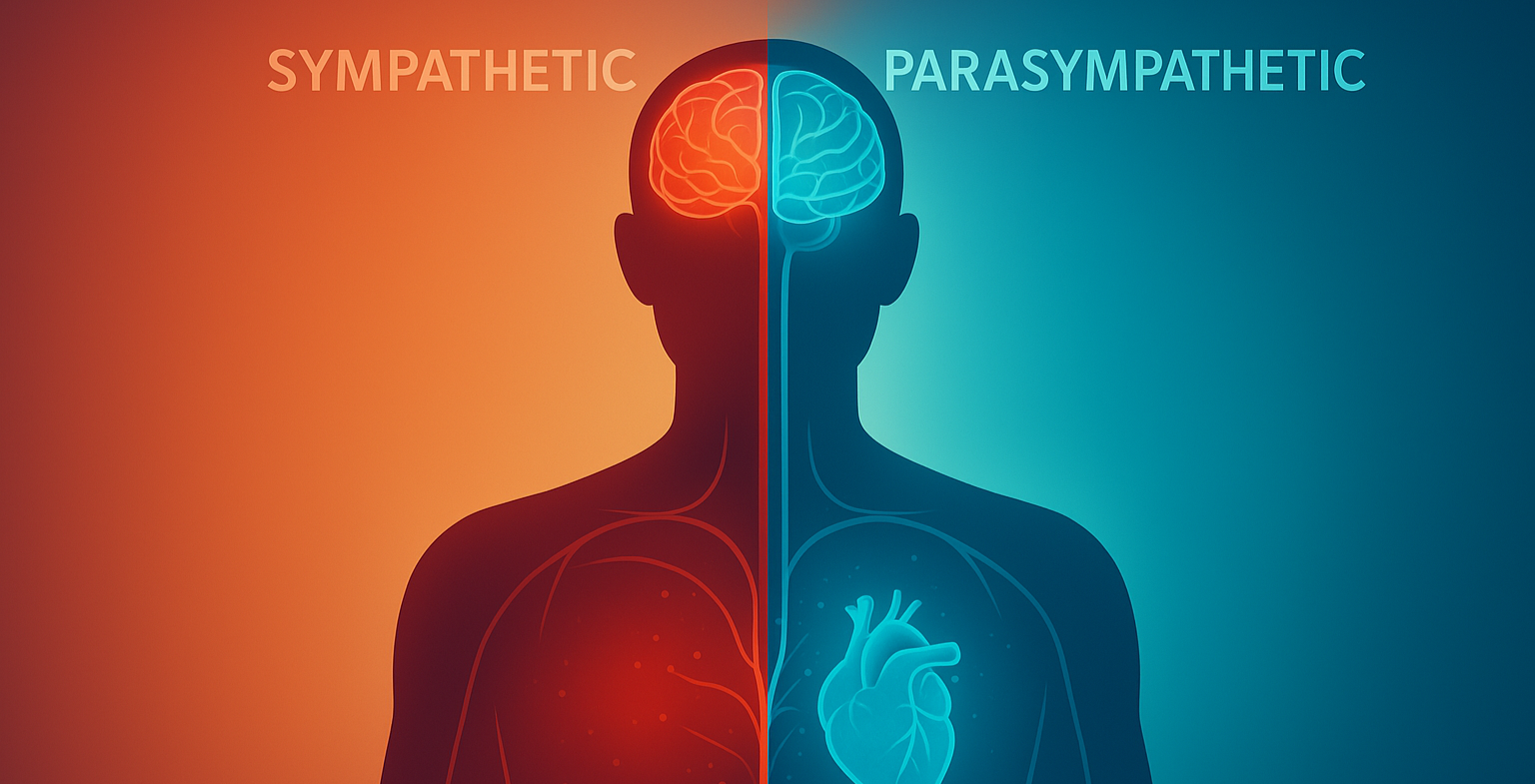
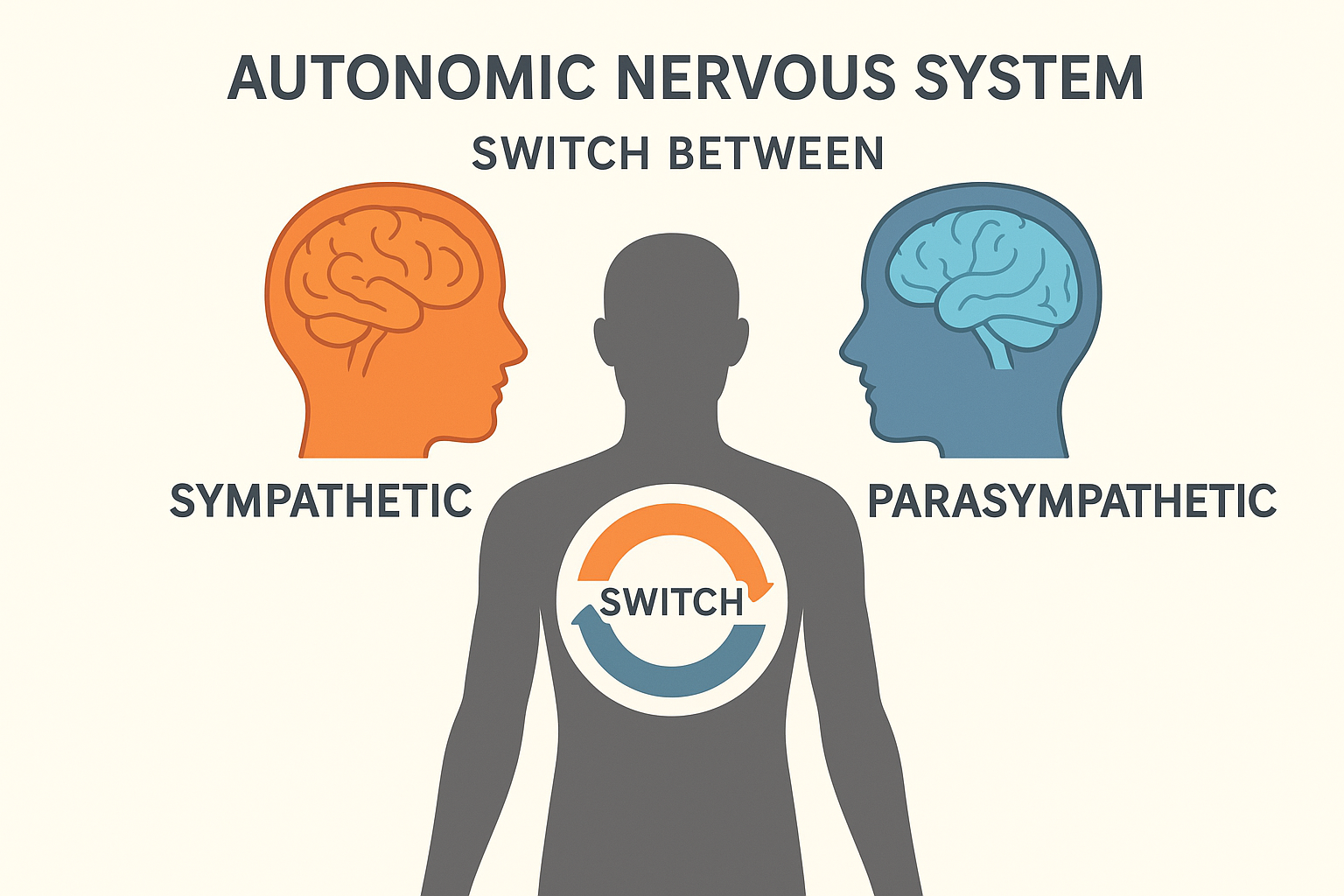
At the nucleus of human performance, mental clarity, and emotional equilibrium lie two opposing yet symbiotic biological systems: the drive for action and the mandate for rest. The first system, our internal accelerator, is governed by the Sympathetic Nervous System (SNS). The second, our sophisticated braking and repair mechanism, is orchestrated by the Parasympathetic Nervous System (PNS). Understanding the dynamic balance between these two forces—a concept known as autonomic flexibility—is the key to unlocking true resilience, sustained energy, and cognitive mastery. They are not independent states but a finely tuned toggle switch, and our ability to control that switch dictates our capacity to thrive in a high-stress world.
The Twin Pillars of Resilience: Activation and Restoration
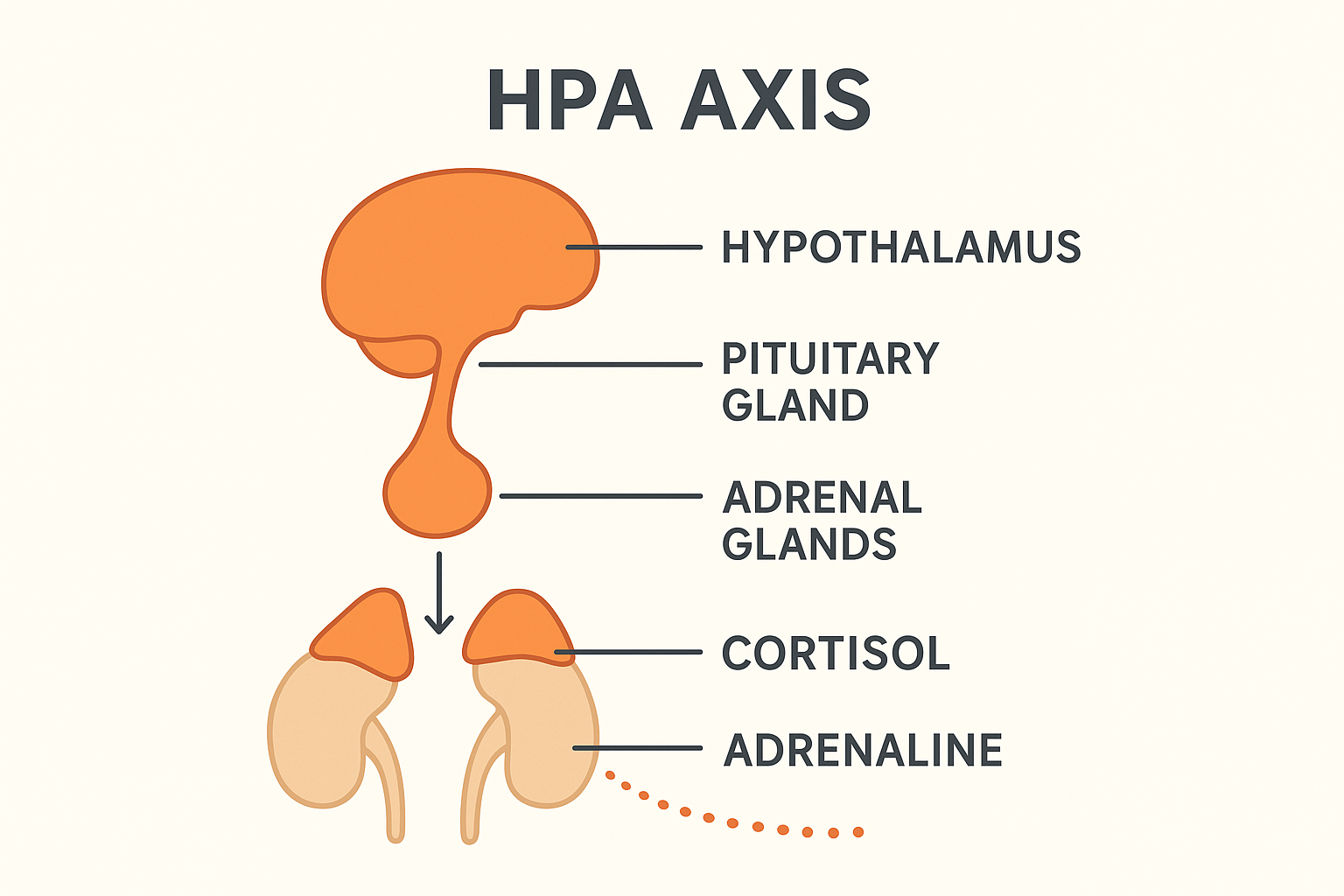
The Sympathetic Nervous System (SNS) is our "fight or flight" engine. When activated by a perceived challenge, it triggers a cascade of physiological responses. This process is initiated by the HPA axis (Hypothalamic-Pituitary-Adrenal axis), the body's central stress response system. The HPA axis signals the adrenal glands to release catecholamines like adrenaline (epinephrine) and cortisol. This hormonal flood mobilizes glucose for energy, increases heart rate, and sharpens focus. This state is essential for high performance, a powerful workout, or meeting a critical deadline.
However, the chronic demands of modern life can cause this system to become "stuck" in the 'on' position. This leads to chronically elevated cortisol, a state of chronic stress, systemic inflammation (low-grade, body-wide inflammation), and burnout, which is a primary driver of modern disease.
This is where the Parasympathetic Nervous System (PNS), the body's ultimate "rest and digest" command, becomes critical. The PNS is governed primarily by the vagus nerve, a massive cranial nerve that wanders from the brainstem to the abdomen, connecting with nearly every major organ. The vagus nerve is the body's main "brake." When activated, it actively counteracts the SNS, releasing the neurotransmitter acetylcholine to slow the heart, promote digestion, reduce inflammation, and shift the body into a state of repair, recovery, and cellular renewal. This dynamic balance, the ability to rapidly engage the SNS when needed and seamlessly shift to the PNS when the challenge is over, is the hallmark of a resilient, high-functioning nervous system.
Forging the Engine: How Hormetic Stress Builds Autonomic Flexibility
Intentional, acute stress is the single most potent tool for training and strengthening this autonomic "switch." Just as lifting weights breaks down muscle to rebuild it stronger, short bursts of physiological stress create a powerful adaptive response in the nervous system. This is the essence of hormesis—a beneficial adaptation resulting from exposure to a mild stressor.
These intentional stressors—such as high-intensity interval training (HIIT), cold exposure (like a cold plunge), or heat stress (like a sauna)—are powerful activators of the Sympathetic Nervous System (SNS). They create a significant, but temporary, physiological crisis. The body's response is not just to return to baseline, but to rebound past it. This rebound involves a powerful, adaptive upregulation of the Parasympathetic Nervous System (PNS) to restore homeostasis.
These intentional stressors—such as high-intensity interval training (HIIT), cold exposure (like a cold plunge), or heat stress (like a sauna)—are powerful activators of the Sympathetic Nervous System (SNS). They create a significant, but temporary, physiological crisis. The body's response is not just to return to baseline, but to rebound past it. This rebound involves a powerful, adaptive upregulation of the Parasympathetic Nervous System (PNS) to restore homeostasis.
This rebound effect trains the nervous system to become more "flexible." It increases vagal tone, which is a measure of the PNS's ability to activate. A high vagal tone is associated with better emotional regulation, lower inflammation, and improved recovery. Over time, this training makes your "brake" more powerful and responsive, allowing you to recover faster from all forms of stress, whether physical or psychological.
The Art of the 'Off' Switch: Directly Activating the Parasympathetic State
While hormetic stress builds long-term resilience, we also need tools to consciously flip the switch from "on" to "off" in real-time. The same nervous system that automatically responds to a threat can also be consciously controlled.
The most direct pathway to activating the Parasympathetic Nervous System is through the breath. Slow, controlled diaphragmatic breathing (where the exhale is longer than the inhale) is a powerful signal to the brain that the body is safe. This breathing pattern physically stimulates the vagus nerve. This connection is so direct it has a biological name: Respiratory Sinus Arrhythmia (RSA). RSA is the natural variation in heart rate that occurs during breathing—the heart speeds up on the inhale (sympathetic) and slows down on the exhale (parasympathetic). By intentionally extending your exhale, you are directly strengthening the parasympathetic braking system.
Practices like meditation and mindfulness function in a similar way. They train the prefrontal cortex to observe thoughts without reacting, effectively uncoupling an external stimulus from an automatic SNS stress response. This creates a "buffer" that allows you to choose your response rather than being a victim of your biology. These practices are not passive; they are active, deliberate training for the parasympathetic "off" switch.
Hacking the System: Measuring Your State with Heart Rate Variability (HRV)
The autonomic nervous system's state is largely controlled by the balance between SNS and PNS inputs. The most effective, non-invasive way to measure this balance is with Heart Rate Variability (HRV).
HRV is not your heart rate; it is the precise measurement of the variation in time between your heartbeats.
A High HRV is a sign of health. It indicates that your nervous system is balanced and highly responsive. Your PNS is dominant, and your heart is "listening" to the inputs from your body, ready to adapt. This signifies a state of "rest and digest," autonomic flexibility, and good recovery.
A Low HRV is a sign of stress. It indicates that your SNS is dominant and your heart is in a rigid, "metronomic" state, ignoring other inputs. It's a clear signal of physical or psychological stress, fatigue, inflammation, or poor recovery.
HRV is the equivalent of a dashboard light for your nervous system. By tracking your HRV (often with a wearable ring or strap, especially upon waking), you can make data-driven decisions. A high HRV reading gives you a "green light" to train hard and push performance. A low HRV reading is a "red light," signaling that your system is stressed and requires active recovery—like breathwork, light movement, or rest—instead of more stress.
The Biohacker's Toolkit
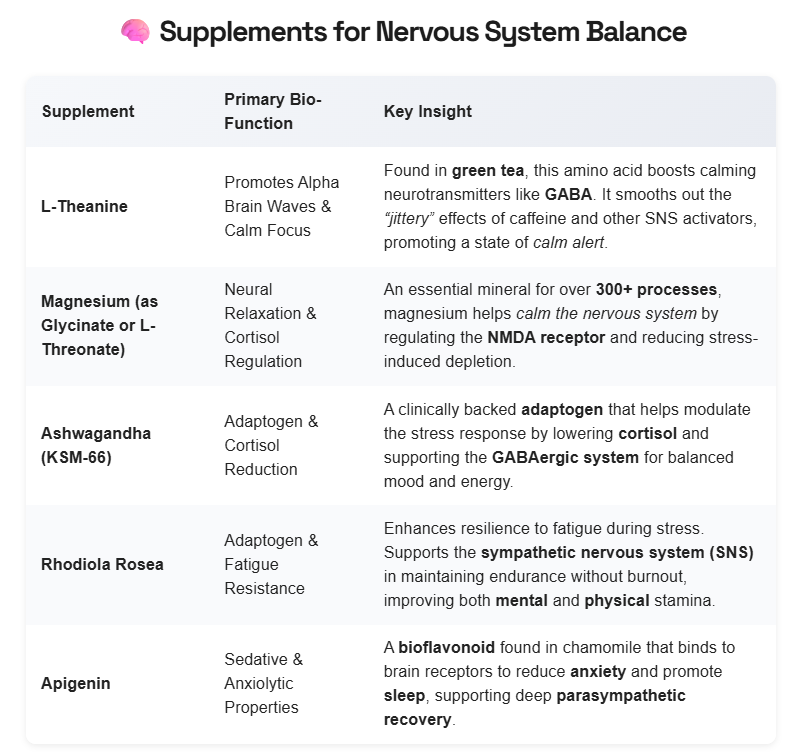
By integrating the hormetic stressors of disciplined training with the conscious, restorative practices of breathwork and meditation, you can take control of your internal "switch." This approach, amplified by targeted nutritional support, allows you to consciously engineer a more resilient, focused, and adaptable biology, laying the ultimate foundation for a longer, healthier, and higher-performing life.
Works Cited
Breit, S., et al. (2018). "Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders." Frontiers in Psychiatry. https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00044/full
Chandrasekhar, K., et al. (2012). "A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults." Indian Journal of Psychological Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC3573577/
Gerritsen, R., & Band, G. P. (2018). "Breath of Life: The Respiratory Vagal Stimulation Model of Contemplative Activity." Frontiers in Human Neuroscience. https://pmc.ncbi.nlm.nih.gov/articles/PMC6137615/
Ishaque, S., et al. (2012). "Rhodiola rosea for physical and mental fatigue: a systematic review." BMC Complementary and Alternative Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC3541197/
Kim, H. G., et al. (2018). "Stress, C-reactive protein, and Heart Rate Variability in U.S. adults." Health Psychology. https://psycnet.apa.org/record/2018-31625-001
Lopresti, A. L., et al. (2019). "An investigation into the stress-relieving and pharmacological actions of an ashwagandha (Withania somnifera) extract." Medicine (Baltimore). https://pmc.ncbi.nlm.nih.gov/articles/PMC6750292/
Pickering, M., & Grgic, J. (2019). "Magnesium and Exercise." Medicina (Kaunas). https://pmc.ncbi.nlm.nih.gov/articles/PMC6683096/
Raut, A. A., et al. (2012). "Exploratory study to evaluate tolerability, safety, and activity of Ashwagandha (Withania somnifera) in healthy volunteers." Journal of Ayurveda and Integrative Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC3487234/
Shaver, J. (2022). "Heart Rate Variability: A Review and Applications for the Study of Stress and Well-being." Frontiers in Psychology. https://www.frontiersin.org/articles/10.3389/fpsyg.2022.879720/full
Stanley, J., et al. (2013). "Cardiac parasympathetic regeneration: a novel strategy to improve autonomic control." Autonomic Neuroscience. https://pubmed.ncbi.nlm.nih.gov/23973641/
Thau, L., & Sharma, S. (2023). "Physiology, Cortisol." StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538239/
White, D. J., et al. (2016). "Anti-Stress, Behavioural and Magnetoencephalography Effects of an L-Theanine-Based Nutrient Drink: A Randomised, Double-Blind, Placebo-Controlled, Crossover Trial." Nutrients. https://pmc.ncbi.nlm.nih.gov/articles/PMC4728665/
Williams, J. L., et al. (2019). "The Effects of Green Tea Amino Acid L-Theanine on Stress and Anxiety in Healthy Adults." Current Pharmaceutical Design. https://pubmed.ncbi.nlm.nih.gov/31758301/